An mpox vaccine has been given provisional approval by Medsafe.
The Government says it has stood up a national-level Incident Management Team to co-ordinate the public health response, and a next step is for the National Immunisation Technical Advisory Group to promptly review which groups are at greatest risk and most likely to benefit from the vaccine.
There are now two confirmed cases of mpox with likely links to the Winter Pride Festival. Investigations are continuing which may result in other cases, but the overall risk of mpox to New Zealand remains low.
The SMC asked experts to comment.
Dr Edwin Reynolds, Medical Advisor, Immunisation Advisory Centre, comments:
“This is very welcome news.
“The access and advertising of the unregistered mpox vaccine product has been quite limiting since 2023 using the specific provision of Section 29. We were unable to advertise vaccine clinics and every vaccine administration required a doctor’s consultation with the resulting prescription for administration.
“The mpox vaccine is being delivered to the most at-risk via sexual health clinics but this announcement means other providers will be able to access the vaccine for their patients.
“Delivery of the vaccine through sexual health clinics to the gay and bisexual community has been a very effective public health tool to prevent ongoing transmission of this virus in the NZ setting.
“Our experience of the vaccine to date is that it is well tolerated with a good safety record so we would encourage those at most risk to receive the vaccine.”
No conflicts of interest.
Note: 12/09/24 This comment has undergone a minor edit for clarification.
Associate Professor Peter Saxton, Director of the Gay Men’s Sexual Health research group, School of Population Health, University of Auckland, comments:
“The current outbreak now has five confirmed cases linked to the Winter Pride Festival in Queenstown, at the time of writing.
“We’re very pleased the vaccine has provisional approval.
“This was a proactive measure by health authorities to get it over the line after two years of limbo. During this time, the vaccine could be offered, but not publicly promoted in New Zealand.
“Now organisations like Burnett Foundation Aotearoa and public health experts can explicitly encourage people most at risk to get vaccinated. In New Zealand, that is men who have sex with men (MSM), and people who have sex with MSM, regardless of gender.
“Encouraging vaccination is important, because mpox vaccine coverage among MSM in New Zealand remains far too low to keep our communities safe. In 2023, our research estimated even one-dose coverage was less than 10% of eligible MSM. Two doses, 28 days apart, is required for optimal protection. Until two-dose vaccine coverage is higher, New Zealand remains at risk of outbreaks every time there’s a new incursion.
“Ongoing incursions of mpox are likely, since we are a globally interconnected community. We still see pockets of transmission internationally from the 2022 pandemic of mpox Clade 2. That affected over 85,000 people over 110 countries, primarily MSM.
“Now the vaccine has been approved, we also recommend emergency resourcing for sexual health clinics around the country, so they can meet demand. Individuals wanting to be vaccinated have reported unacceptably long waiting lists. Timely immunisation is key to stopping spread.
“While stepping up a targeted vaccine programme requires a small up-front investment, prevention by vaccination, testing, and contact tracing helps avert a much wider local outbreak. That in turn is cost-effective, avoids overwhelming health services, and frees up care for others.
“Like all prevention programmes, it can pay big future dividends.
“We also commend the gay and bisexual men who have sought testing and vaccination in relation to the current outbreak. Some have bravely gone public with their experiences, showing there is no room for stigma in managing infectious diseases like mpox.
“Although MSM remain at disproportionate risk in Aotearoa New Zealand, mpox can affect anyone.”
No conflicts of interest.
Associate Professor Helen Petousis-Harris, Faculty of Medical and Health Sciences, University of Auckland, comments:
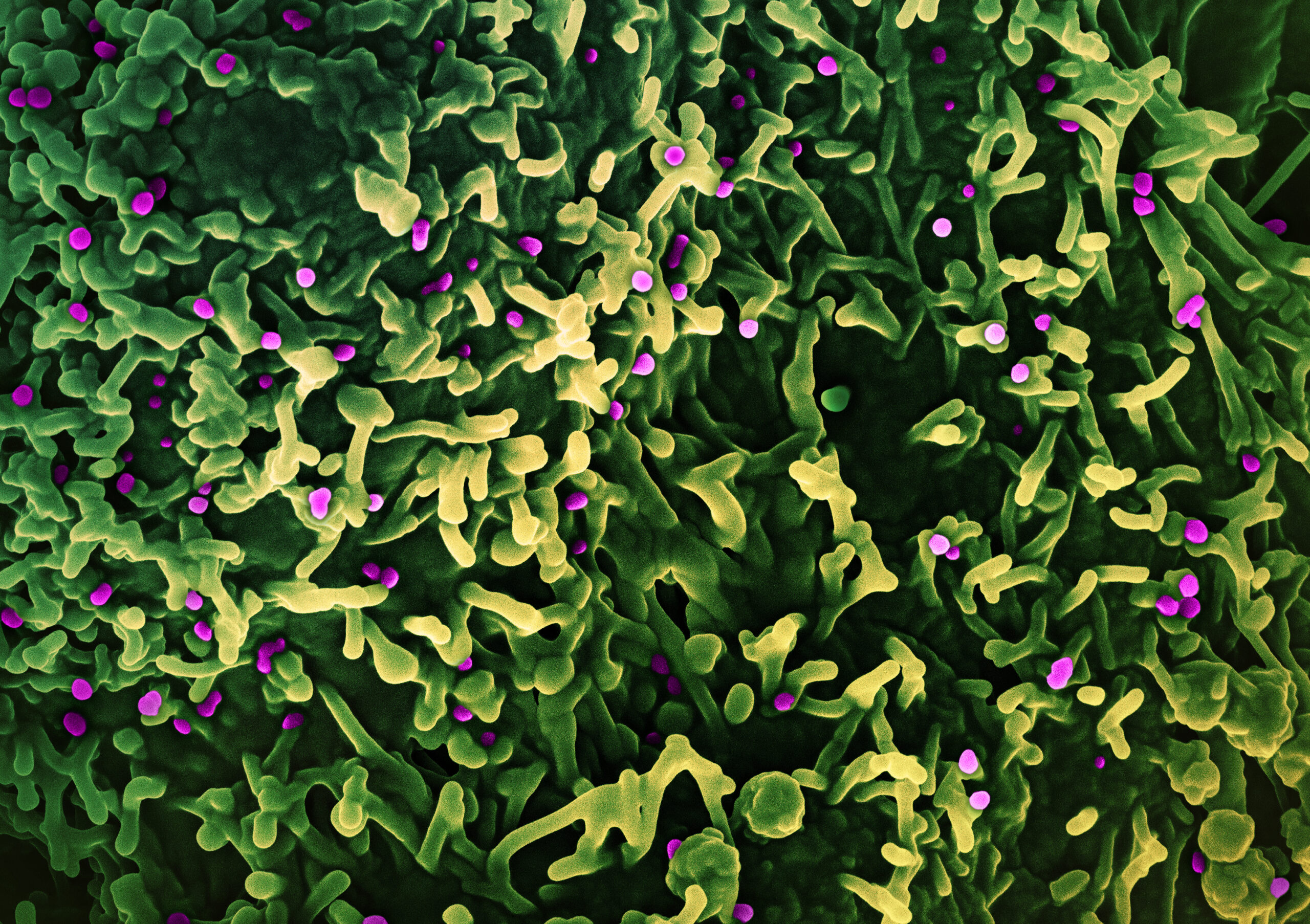
“For several years mpox has been increasingly diverging from its previous distribution in Central and West Africa to cause outbreaks globally. Changes to the viral genome mean it is better able to spread. It is clear that mpox is becoming a growing threat to public health. This is an example of how neglected problems in one part of the world can affect everyone.
“It is spread through close contact with an infectious person or contaminated materials or infected animals. We are fortunate to have several vaccines globally. The vaccine available in NZ is called JYNNEOS and it is made by a company called Bavarian Nordic in Norway. This is a live vaccine but is not able to replicate.
“Here’s a breakdown of what we know about the effectiveness of JYNNEOS:
“Protection against MPOX:
- Before exposure: In people vaccinated before exposure to the MPOX virus, JYNNEOS is believed to provide solid protection. Clinical trials indicated that JYNNEOS generates a strong immune response, with the immune markers suggesting it offers good protection against both MPOX and smallpox (as the vaccine is primarily derived from a modified vaccinia virus, related to both).
- Post-exposure: JYNNEOS can also be used as post-exposure prophylaxis (PEP). When administered within 4 days of exposure, it is expected to prevent the onset of disease. If given between 4 to 14 days after exposure, the vaccine may reduce the severity of symptoms, though it might not prevent the disease entirely.
“Effectiveness Estimates:
- During the 2022 MPOX outbreak, studies indicated that people who received one dose of the JYNNEOS vaccine were around 30–50% less likely to get infected compared to unvaccinated individuals.
With two doses, effectiveness improved, with early studies suggesting that fully vaccinated individuals (with both doses) could have up to *66–85% effectiveness in preventing infection.
“Timing of Protection:
- Optimal protection is expected about 2 weeks after the second dose of the JYNNEOS vaccine, which is given as a two-dose series (the second dose administered 28 days after the first).
“Milder Disease in Vaccinated Individuals:
- Even if vaccinated individuals contract MPOX, the disease is often milder and less severe compared to unvaccinated individuals. This reduced severity helps lower the risk of transmission and serious complications.
“Real-world Data:
- Data from the 2022 outbreak has shown that people who were fully vaccinated (two doses) were significantly less likely to contract MPOX and had fewer severe symptoms when compared to unvaccinated people
“The vaccine has a strong safety profile, with mostly mild side effects and a low risk of severe adverse reactions. It’s particularly well-tolerated across a wide range of populations, including those with compromised immune systems.
“JYNNEOS provides good protection against MPOX, especially after the second dose, and also helps reduce the severity of disease. However, breakthrough infections can occur, so it’s essential to combine vaccination with other protective measures in outbreak settings.
“Hopefully everyone at risk of MPOX infection will be able to access vaccine, this includes people in Africa who have the greatest need.”
Conflict of interest statement: No conflicts of interest related to mpox or mpox vaccines.
Professor Michael Baker, Department of Public Health, University of Otago, Wellington, comments:
“It is positive to see Government and health authorities taking a proactive approach to managing the threat posed by mpox within Aotearoa New Zealand.
“The recent media release mentions several valuable steps, including a mechanism to coordinate the response, improved communications, and increased vaccine access. It will be important to monitor the response to this epidemic and ensure that measures such as vaccination are reaching those who are at highest risk of mpox infection.
“Aotearoa New Zealand should also review its overseas aid contribution and support for programmes that could assist prevention and control of the severe mpox epidemic in Africa. Doing that would also support global control of this health emergency.”
No conflicts of interest.
Associate Professor Mark Thomas, Molecular Medicine and Pathology, University of Auckland, comments:
“Monkey pox, also known as mpox, is very closely related to several other pox viruses, including smallpox, cowpox and camelpox. Infection with each of these viruses provides protection against subsequent infection with any of the other closely related pox viruses.
“Deliberate inoculation of a small amount of cowpox virus, the original meaning of the term “vaccination”, was shown by Edward Jenner in 1757 to provide strong protection against infection with smallpox, which at that time was responsible for the deaths of about one person in five in most European nations. Various cowpox vaccines have been developed in recent years, to ensure that the people in military institutions who maintain the stocks of smallpox virus for potential use as biological weapons, are immune to infection from smallpox. These vaccines have provided a fortunate resource for use in the control of mpox outbreaks.
“The JYNNEOS vaccine that has been given provisional approval by Medsafe for use in New Zealand contains a mutant form of the cowpox virus. When the mutant cowpox viruses in the JYNNEOS vaccine are injected they enter the cells of the vaccinated person where they undergo one cycle of replication, but the progeny viruses lack the ability to undergo further replication. The result is that people who receive this vaccine cannot have the repeated cycles of replication that would be required either for severe cowpox disease, or for transmission of cowpox virus to another person. The vaccine is therefore safer than other earlier cowpox vaccines.
“Immunisation with the JYNNEOS vaccine requires two doses administered four weeks apart. Vaccine efficacy, against mpox disease in people in developed nations, is approximately 76% after one dose and 82% after two doses. Vaccination given after exposure to the mpox virus provides much less protection against disease, with vaccine efficacy in this context of approximately 20%.
“Vaccination should be encouraged for people who consider themselves at significant risk of mpox infection in the future. Vaccination is not required for people who have suffered an episode of mpox, they are likely to have lifelong immunity.”
No conflicts of interest.