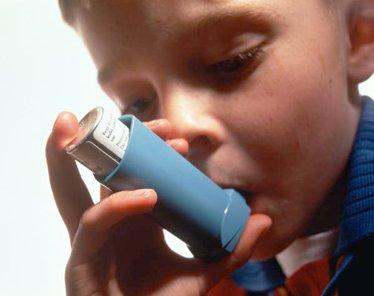
Overweight women who become pregnant could be putting their children at risk of developing asthma in their teens, research released today suggests.
 From the BMJ abstract:
From the BMJ abstract:
Background The high prevalence of children’s asthma symptoms, worldwide, is unexplained. We examined the relation between maternal pre-pregnancy weight and body mass index (BMI), and asthma symptoms in adolescents.
Methods Data from 6945 adolescents born within the Northern Finland Birth Cohort 1986 were used. Prospective antenatal and birth outcome data, including maternal pre-pregnancy weight and BMI, and asthma symptoms in adolescent offspring at age 15-16 years, were employed. Logistic regression analyses were performed to examine the associations between relevant prenatal factors and asthma symptoms during adolescence.
Results Current wheeze (within the past year) was reported by 10.6% of adolescents, and physician-diagnosed asthma by 6.0%. High maternal pre-pregnancy BMI was a significant predictor of wheeze in the adolescents (increase per kilogram per square metre unit; 2.7%, 95% CI 0.9 to 4.4 for ever wheeze; 3.5%, 95% CI 1.3 to 5.8 for current wheeze), and adjusting for potential confounders further increased the risk (2.8%, 95% CI 0.5 to 5.1; 4.7%, 95% CI 1.9 to 7.7, respectively). High maternal pre-pregnancy weight, in the top tertile, also significantly increased the odds of current wheeze in the adolescent by 20% (95% CI 4 to 39), and adjusting for potential confounders further increased the risk (OR=1.52, 95% CI 1.19 to 1.95). Results were similar for current asthma. Furthermore, these significant associations were observed only among adolescents without parental history of atopy but not among those with parental history of atopy.
Conclusions The association demonstrated here between maternal pre-pregnancy overweight and obesity, and asthma symptoms in adolescents suggests that increase in asthma may be partly related to the rapid rise in obesity in recent years.
Our colleagues at the UK Science Media Centre gathered reaction from scientists to the journal paper, which is published in the Journal of Epidemiology and Community Health.
Professor Andrew Prentice, Director of MRC International Nutrition Group at the London School of Hygiene & Tropical Medicine, said:
“In studies of associations between certain risk factors (in this case a mother being overweight before and during pregnancy) and outcomes (in this case asthma when their children reached adolescence) it is notoriously difficult to be certain that the one leads directly to the other – they might both be caused by so-called ‘bystander’ effects. The authors have done their best to account for such effects but we cannot be certain that maternal obesity causes asthma.
“There are many possible pathways by which a mother being overweight in pregnancy could alter the development of her baby and make it more susceptible to later diseases. Therefore Patel’s results are plausible and should be followed up by a search for the actual mechanism so that interventions could be planned.
“These new findings add to a very long list of the damaging effects of obesity in pregnancy. Overweight mothers not only put themselves at risk, but also their unborn babies and, almost certainly, their grandchildren. The costs to our health service are enormous and responsibility lies at a societal level as well as with the individual.”
Dr Alexander Heazell, Walport Clinical Lecturer at the University of Manchester’s School of Medicine, said:
“Obesity is already associated with an increased inflammatory state in pregnancy which may affect foetal development. This research provides more data to support a link between maternal obesity and childhood asthma. The authors found that women in the top third of pre-pregnancy weight were more likely to have a teenage child with asthma. There was a trend towards increased asthma in women classified as obese, but this was not statistically significant, probably because only 3.8% of women were obese in this study. Maternal weight was not the only predictive factor; there are still other important genetic and environmental considerations.
“This adds to a growing body of data that show what happens in the womb can determine the future health of the child. Until now, most work has focussed on maternal under-nutrition which increases the risk of diabetes and cardiovascular disease in offspring. This work suggests that women with obesity can predispose their child to health problems in utero. Optimising maternal health before embarking on pregnancy should be a priority. ”
Professor Khalid Khan, Professor of Women’s Health and Clinical Epidemiology, Barts and the London School of Medicine, said:
Background:
“The increasing prevalence of obesity in women is a major health problem: a recent Health Survey for England showed that a quarter of women (23.8%) were obese with a Body Mass Index (BMI) of 30 kg/m2 or more. Fifty percent of women of childbearing age are either overweight (BMI 24.9-29.9 kg/m2) or obese with 18% starting pregnancy as obese. Currently 20-40% of women are found to gain more than the recommended weight during pregnancy. They have an increased risk of maternal complications, e.g. more than half of women who die during pregnancy, childbirth or puerperium are either obese or overweight. There are also many risks to new-born and children, e.g. excessive weight gain in pregnancy increases the risk of obesity in children at 2-4 years. The risk of asthma in adolescent offspring of obese women has been evaluated in the study.
Childhood Asthma:
Prevalence of children’s asthma symptoms has been on the increase in recent decades with up to a third (37%) of teenagers affected by asthma symptoms, making it one of the most common chronic diseases in childhood. The reasons for this rise are difficult to decipher, in part due to variation criteria for diagnosis over time. As with most diseases, a mixture of genetic susceptibility and environmental factors contribute. The extent to which each contributes varies. It is thought that genetic variation is unlikely to be the key reason for the risk in childhood asthma. So what has changed in the environment?
Prenatal environment:
The exposure of the foetus while still in utero is a considered a key factor in current research, e.g. it has been shown that exposure to frequent use of paracetamol during late pregnancy may increase the risk of persistent wheezing in the offspring in early childhood. Smoking in pregnancy has the same effect on the offspring. This study shows that maternal pre-pregnancy overweight and obesity are associated with asthma symptoms in adolescents. The epidemic of obesity in women of childbearing age may provide a partial explanation for the increase in childhood asthma.
Threats to validity of this study:
Observational studies of the kind reported in this paper provide possible explanations, nothing more and nothing less. Their findings can be spurious due to inherent biases arising from the way data are collected or analyses carried out. For example in this study the effect of paracetamol exposure was not adjusted for. Thus these studies tend to fall short of providing strong evidence for informing public health policies. For this, randomised studies would be required.
Implications for practice and policy:
Pregnancy offers the opportunity to intervene for the prevention of obesity with the aim of reducing maternal and foetal morbidity and mortality. Whilst reduction in weight gain or weight loss may be of benefit there is a potential for harm to mother or baby due to weight loss itself or due to the interventions. There are many randomised controlled trials of weight management interventions in pregnancy. The offspring from these trials should be followed up to see if the reduction of maternal obesity achieved through intervention leads to reduction in asthma. Moreover what is required is an evidence synthesis of these randomised studies to allow balancing of risks and benefits in quantifiable terms.”
* ‘Associations between pre-pregnancy obesity and asthma symptoms in adolescents’ by Swatee Patel et al. was published in the Journal of Epidemiology and Community Health