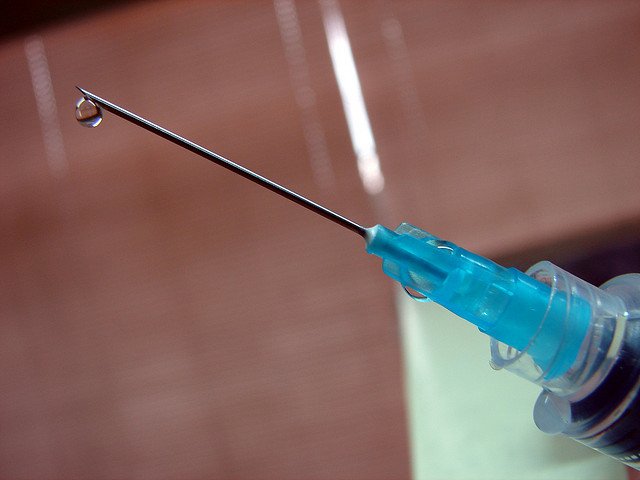
New international research indicates that just one dose of the Cervarix HPV vaccine – currently unavailable in New Zealand – could prevent the majority of cervical cancers.
UPDATE: New comment below.
Vaccination against human papillomavirus (HPV) can protect against infection and the risk of developing cervical cancer and a range of other HPV related diseases later in life.
A new combined analysis of two independent trials, published today in The Lancet Oncology, suggests that young women who received three, two, or one dose of the Cervarix vaccine were equally protected against infection by particular HPV variants for at least four years after vaccination.
“Our findings question the number of HPV vaccine doses truly needed to protect the majority of women against cervical cancer, and suggest that a one-dose schedule should be further evaluate,” said study author Dr Aimée Kreimer from the National Cancer Institute (NCI), National Institutes of Health, USA.
“If one dose is sufficient, it could reduce vaccination and administration costs as well as improve uptake.”
New Zealand’s HPV Immunisation Programme uses a three dose schedule of the Gardasil vaccine. It is free for girls and young women up to their 20th birthday.
The Science Media Centre contacted experts for comment.
NEW COMMENT: Dr Helen Petousis-Harris, Director of Immunisation, Research and Vaccinology at the University of Auckland’s Immunisation Advisory Centre, comments:
“I am not surprised a single dose of the Cervarix vaccine as been demonstrated to be so immunogenic. This vaccine has a different formulation to the Gardasil vaccine. It uses a different adjuvant (immune enhancer). The Cervarix vaccine generates more antibodies that the Gardasil vaccine – it appears to be slightly more immunogenic.
“In New Zealand we use the Gardasil vaccine. The key difference between the two vaccines is that while Cervarix provides protection against cervical and other cancers, Gardasil also provides protection against genital warts.
“Studies have demonstrated that Gardasil is also effective with fewer doses in young women and moving to a two dose schedule may be something New Zealand will consider.
“If NZ moved to using Cervarix we would lose the protection against genital warts.
“These are both extremely effective vaccines against cervical cancer.”
Assoc Prof Nikki Turner, Director, Immunisation Advisory Centre, comments:
Should New Zealand switch from three dose Gardasil to one dose Ceravrix?
“In terms of moving to the bivalent vaccine (Cervarix) the disadvantage is that while it covers the same two types of HPV that are the most common underlying causes of cervical cancer it does not contain the other two serotypes that Gardasil contains – these two are the most common cause of genital warts. Both Australian and NZ data have shown dramatic reductions in genital warts since the introduction of Gardasil.
“This is hugely effective and in fact there is some discussion as to whether it would be possible to even eradicate genital warts. So I think NZ would be reluctant to move away from a quadrivalent vaccine with the evidence we have to date on the effectiveness of Gardasil.
“I am a member of the WHO SAGE committee who looked at HPV vaccines dosages last year and recommended that the quadrivalent vaccine (ie Gardasil) could be given to those under 15 years in a two dose regime. This data has been presented to the NZ PITAG subcommittee to Pharmac and the recommendation is for NZ to move towards using a two dose regime in girls under 15 years of age.
“We are awaiting further news as to whether this will get recommended by Pharmac and the Ministry of Health. Personally I think there would be considerable advantage in being able to deliver a two dose rather than a three dose regime in terms of making it easier to deliver in our school based programmes. The reason for recommending a two dose regime to those only under 15 years is that the younger adolescents show a more vigorous response than older adolescents to the vaccine, so there appears to be an advantage to vaccinating at a younger age”
Commentary from the UK SMC:
Dr Vanessa Saliba, PHE Consultant Epidemiologist, comments:
“The Human Papillomavirus(HPV) immunisation programme for adolescent girls was introduced in England in 2008 with the aim of reducing the incidence of cervical cancer in women. School-based HPV immunisation delivery has successfully achieved high coverage for the full three-dose course which has been consistently above 86% over the last three years.
“In March 2014, based on the latest immunological evidence, the Joint Committee on Vaccination and Immunisation (JCVI) advised a change from a three to a two-dose schedule in the routine programme, which was implemented in September 2014. The HPV vaccine used routinely in the national programme in England when it started was Cervarix, which protects against HPV types 16 and 18, which are responsible for over 70% of all cervical cancers in Europe. This was changed to Gardasil in September 2012, which in addition protects against a further two strains of HPV – types 6 and 11 – that cause the vast majority of genital warts.
“While The Lancet Oncology study is encouraging, we look forward to further research being conducted into HPV vaccine dosage to confirm these results. JCVI continues to keep the HPV immunisation programme under review and will consider this new evidence in due course.”
Prof Margaret Stanley, Professor of Epithelial Biology and Director of Research of the Department of Pathology, University of Cambridge, said:
“The paper from Kreimer and colleagues reporting data from a post hoc analysis of two trials with the bivalent HPV vaccine Cervarix that suggests that even one dose of a VLP vaccine provides equivalent protection against infection with HPV 16 and 18, the most important of the cancer causing HPVs, could be the game changer for the implementation and uptake of these vaccines worldwide. Delivering one dose rather than two or three would be easier in settings with little medical infrastructure and crucially cheaper, not just in vaccine costs but delivery costs.
“However there is still a way to go before one dose vaccination could even be considered for introduction. As Kreimer and colleagues point out themselves, this is a post hoc analysis, the numbers are small and the measure of efficacy is not disease but infection and incidence rather than persistent infection. Nonetheless the striking data in this study support the calls for clinical trials that assess the efficacy of one dose of HPV vaccine in women and men. These are unlikely to be sponsored by the manufacturers of these products but because of the overwhelming public health importance of this question should be a priority for national and international funding agencies.”
Dr Mark Jit, Senior Lecturer in Vaccine Epidemiology, London School of Hygiene & Tropical Medicine, said:
“Many countries including the UK recently switched from giving three doses to giving two doses of the HPV vaccine to girls up to 14 years old. This followed findings from Costa Rica and other studies that two doses of vaccine may be enough to protect women from cervical cancer. The latest news that even one dose may be protective holds promise, although further studies are needed before we will be ready to consider a one dose schedule.”