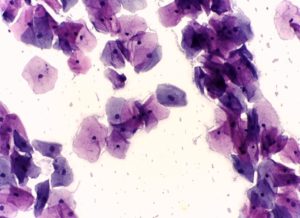
An Australian study has found that human papillomavirus (HPV) testing detects a higher number of precancerous cervical lesions than traditional Pap smears.
Many countries are considering switching from the classic Pap smear to HPV testing for cervical cancer screening. From 2018, New Zealand’s National Cervical Screening Programme (NCSP) will change the first step in the screening process to an HPV test.
The SMC gathered expert reaction to the study, please feel free to use these comments in your reporting.
Associate Professor Peter Sykes, Obstetrics and Gynaecology, University of Otago, comments:
“This is an important study performed in a context that can be readily compared to the New Zealand National Cervical Screening Programme (NCSP). It confirms that HPV testing offers a greater sensitivity for the detection of precancerous cervical abnormalities than cytology screening tests and supports the NCSP decision to change to this method of screening. It also offers useful information for the NCSP regarding what may be expected with regard to changes in referrals due to an abnormal test.”
Conflict of interest statement: I have received research grants from Roche in the past and have provided some clinical advice to a substudy of the reported study performed in Auckland. Neither of these are current.
Associate Professor Brian Cox, Hugh Adam Cancer Epidemiology Unit, University of Otago, comments:
“This study suggests that the change to HPV screening in New Zealand is likely to require a 40% increase in colposcopy services that will not be offset by HPV vaccination. The study found that, in Australia, colposcopy referral when using HPV screening was high even in women offered HPV vaccination. Colposcopy referral was also much higher than for current cytology screening whether or not women had been offered HPV vaccination.
“In this previously screened population, a population for which most cytology-detectable abnormalities are likely to have already been found, further cervical neoplasia was detected by HPV screening. However, as only a minority of cervical neoplasia progresses to invasive cancer, it is not known whether the additional disease detected was likely to progress or not.
“Two of five longer-term randomized trials have not found an increased incidence of invasive cervical cancer with HPV screening compared to current cytology screening and the impact of HPV screening on cervical cancer incidence is yet to be established.”
No conflict of interest.
Professor Ann Richardson, cancer epidemiology, University of Canterbury, comments:
“The paper by Canfell et al reports findings of the Compass Trial, where the screening results for women who had been randomly assigned to three different cervical screening approaches were compared.
“The three screening approaches were (1) cytology screening (2) HPV screening, with women identified with HPV types 16 or 18 referred to colposcopy, and cytology for other high-risk HPV types, and (3) HPV screening, with women identified with HPV types 16 or 18 referred to colposcopy, and dual-stained cytology for other high-risk HPV types.
“Referral rates for colposcopy were higher in the HPV groups than in the cytology group, but the differences were not statistically significant (a concern about HPV screening has been that too many women would be referred to colposcopy).
“Rates of pre-cancer detected in the two HPV groups were statistically significantly higher than in the cytology group (about 1.0% for women in each of the HPV groups compared with 0.1% for women in the cytology group).
“The authors reported that the higher detection rates for HPV screening compared with cytology screening were also found in younger women who had been offered HPV vaccination (although the difference was of borderline statistical significance).
“The women in the trial were at low risk (women undergoing follow-up because of previously abnormal smears had been excluded) so the referral rates and pre-cancer detection rates are likely to have been lower in this trial than in a screening programme.
“With respect to screening in New Zealand:
“The screening approach for group 1 in this trial is similar to the current cytology screening programme in NZ, while the screening approach for group 2 in the trial is similar to the proposed HPV screening programme for NZ.
“HPV vaccination coverage is higher in Australia than in NZ. In Australia, coverage of women offered vaccination is about 50-77%, whereas in NZ it is about 48-56% nationwide.
“HPV vaccination reduces the risk of developing pre-cancer of the cervix, so increasing HPV vaccination should be a priority.”
No conflict of interest.
Dr Peter Fitzgerald, cytopathologist, Southern Community Laboratories, comments:
“The Compass pilot study results show that HPV screening overall increased colposcopy referrals in a selected (low risk) Victorian population by 40% compared to cytology screening. In young women, the colposcopy referral rate for HPV (8.1-8.9%) was nearly double that of cytology (4.7%). This is only a pilot and we must wait for better information from the main study.
“There are a number of issues with the pilot study data; the numbers in the 3 study arms are small, vaccination percentages are an estimate as there is no individual vaccination data, the vaccinated population is at most 20% of the total population, there is no mechanism to adjust for verification bias and 2 different HPV tests are used.
“But of particular note is the extremely low rate of HSIL (0.1%) in the cytology study arm. This low figure is hard to understand as it is so much lower than the routine Victorian screening HSIL rate. The low cytology HSIL detection rate triggered the investigators to send the Compass cytology to another laboratory to check the results. This is unusual.
“Most surprisingly it seems no HSIL was identified in the 65 women in the LBC arm who had low grade cytology even though the HRHPV positive rate for these women was 66%. NZ data would predict 20% of low grade cytology will on triage have HSIL. In NZ, 65 women with low grade cytology would on further follow up (triage) have 13 more HSIL. In the Compass study there did not appear to be any additional HSIL in the low grade women, why?
“The explanation given is that the study population is low risk. If that is true it makes extrapolating the Compass pilot data to NZ difficult. The most recent NZ cytology data, which now also represents a partially vaccinated population, has a cytology detected HSIL rate over 10x higher than Compass at 1.1% v 0.1%. The Compass study and NZ are different populations. The NZ population (2016) has a much higher level of cytology detected HPV related abnormalities (HSIL) than Victoria (2014).
“The Compass data shows that HPV screening increases test sensitivity in Victoria and even in a population with a low rate of cytology detected HPV related abnormalities (HSIL) the numbers of colposcopies will increase by 40%. The NZ population has a significantly higher rate of cytology detected HPV related abnormalities (HSIL) than the Compass pilot study, if HPV test sensitivity is increased as predicted the increase in colposcopy referrals will be greater than seen in the Victorian Compass study.”
Conflict of interest statement: I am a cytopathologist, employed by Southern Community Laboratories (SCL). SCL has a contract to provide laboratory services to the NCSP (HPV, cytology, histology and microbiology). SCL is NZ’s largest provider of HPV, cytology and histology tests to the NCSP. I have particular expertise in the area of cytopathology. I have a long-standing interest in the role of new technologies in cervical cancer screening. I do not have any conflicts of interest with respect to my comments on cervical cancer screening and the choice of the best test platform(s).