New Zealand, alongside the rest of the world, is having to make unprecedented policy decisions in the face of the COVID-19 pandemic. What’s the evidence behind it?
The SMC asked experts to comment on the evidence behind taking strict quarantine measures to curb the spread of the virus, and how researchers should cope with the breakneck speed of research coming out on the topic.
Dr Ayesha Verrall, Senior Lecturer, Department of Pathology and Molecular Medicine, University of Otago, Wellington, comments:
“Evidence for quarantine is centuries old. I’m not aware of any new evidence for this but would be happy to discuss.
“Pre-print articles haven’t been through peer review, so they might contain errors, particularly with respect to how the data are presented and interpreted. Essentially, I read them extra carefully, and sometimes will seek a colleague’s view on an aspect that looks suspicious. The media should always get expert commentary from someone other than the study author.
“[Regarding the case fatality rate for the 2009 swine flu] the people who showed up in the official statistics had severe disease and sought medical help. After the outbreak scientists can survey large parts of the community and perform blood tests to check for antibodies. This revealed more people had had the swine flu than initially thought. They probably had mild illness and did not seek care. When you discover there were many more cases this reduces the ratio of deaths to cases.
“I think most infectious diseases epidemiologists know the case fatality ratio in an outbreak is likely to be overestimated, and when modelling outbreaks you always use a range of plausible values. You should also look at data from a variety of different contexts when you look at a case fatality rate.”
Conflict of interest statement: Dr Verrall is the deputy chair of Capital and Coast DHB.
Professor Shaun Hendy, University of Auckland, comments:
“COVID-19 is a new disease, so we are learning about it all the time. There are hundreds of new papers coming out every day and modellers are doing their best to keep up with the latest clinical data, which is becoming more robust as we learn more. While papers are not going through traditional peer review, which can take many months, most receive some form of peer review. The New Zealand modelling papers have been reviewed by the Ministry of Health or by other colleagues.The Otago and Te Pūnaha Matatini modelling groups have exchanged work so that we can understand any differences in scenario outcomes, but it is important to realise that the groups have been exploring different scenarios.
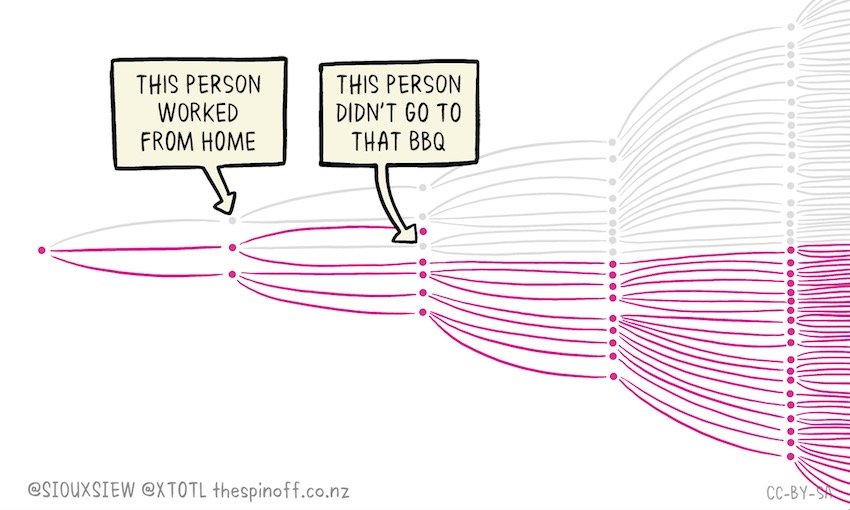
“Control measures are also changing, as many countries implement control measures, and modellers are doing their best to take this into account. For this reason we should expect to see variations in the scenarios that the models explore. In New Zealand, the models consistently show that without action the healthcare system would be overwhelmed and tens of thousands will die. But now that the Alert Level 4 measures are in place, the size and timing of any model will depend on when the modellers assume that the government will relax those measures as well as how effective the researchers think they might be. The longer we can delay any peak with these measures, the more prepared our healthcare system will be, which means that more people will receive the best care.
Conflict of interest statement: Prof. Hendy has been seconded to the National Crisis Management Centre.
Professor Robert G. Webster, Emeritus faculty, Division of Virology, Department of Infectious Diseases, St. Jude Children’s Research Hospital, USA, comments:
“Quarantine and social distancing are the only options available when a novel infectious disease emerges to which there is no vaccine and no medicine. These strategies together with reliable testing have enabled South Korea to emerge from lockdown but they are aware of a possible second wave and are testing it.
“It is important to share information as quickly as possible in the face of a new emerging infectious disease, always keeping in mind the possibility of non-validated information. Fortunately, science is self-regulating and misinformation or fraudulence is relatively quickly revealed.
“As I remember the case fatality rate for the 2009 swine flu did not change. There was a higher fatality rate in some ethnic groups in the world including ethnic groups in Canada and Australia, but overall the fatality rate was relatively low as compared with the Asian flu pandemic of 1957 and the Hong Kong flu pandemic of 1968.”
No conflict of interest.
Professor Mick Roberts, Professor in Mathematical Biology, Massey University, Auckland, comments:
“You need to calculate the number of deaths due to COVID-19 divided by the number of cases of COVID-19. The number of deaths is the numerator. At first glance to number of deaths looks easy to obtain. But, with older people the question is ‘Did they die because of COVID-19 or did they die with COVID-19?’ There are also patients with COVID-19 that may, unfortunately, succumb in the future.They are missing from the current inventory.”So much for the numerator, what about the denominator – the number of cases. The case definition is often revised, so the number of cases may change as the definition changes. There is often confusion between the Case Fatality Ratio (CFR) and the Infection Fatality Ratio (IFR). If there are a number of infected people with mild or no symptoms, or who do not for other reasons become recorded as a case, then these ratios are very different. The CFR is the proportion of cases (according to the current definition) that lead to a fatality. The IFR is the proportion of those who are infected with COVID-19 that die due to the infection. Where there are a number of people with mild symptoms, the number infected is not recorded. The IFR will always be less than the CFR.”
No conflict of interest.