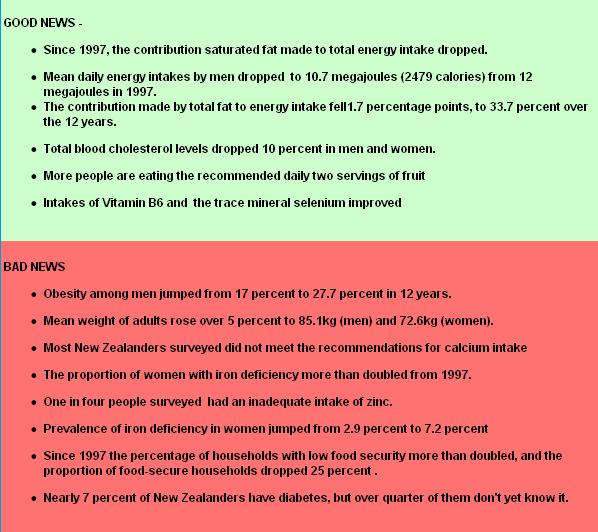
New Zealand’s latest nutrition survey shows the nation’s obesity epidemic surged ahead over the past dozen years — even though the population’s energy intake levels have dropped.
 Researchers who conducted the 2008-2009 Adult Nutrition Survey (NZANS) say they suspect this means many people are exercising less than they did when the comparable 1997 National Nutrition Survey was carried out.
Researchers who conducted the 2008-2009 Adult Nutrition Survey (NZANS) say they suspect this means many people are exercising less than they did when the comparable 1997 National Nutrition Survey was carried out.
The report on the survey’s key findings titled, A Focus on Nutrition, was released Thursday 15th September 2011.
The survey found that the prevalence of obesity among men jumped from 17 percent in 1997 to 27.7 percent in 2008-2009 and from 20.6 percent in women to 27.8 percent.
Among Maori, 40.7 percent of men were obese, and 48.1 percent of women. Obesity is a factor in many health problems ranging from cardiovascular disease through some types of cancer and diabetes to psychological illnesses. In a 2004 report, Tracking obesity, the Ministry of Health reported that the “epidemic of obesity” began before the 1970s and that by 1977 9 percent and men and 11 percent of women were obese.
Results from the survey, by Otago University and Health Ministry researchers, will be used by policymakers, and will help develop Government food and nutrition guidelines. Thy may also be used in monitoring diabetes, developing food standards, and watching changes in the food supply.
FACTBOX
The Science Media Centre has prepared further analysis of the survey’s results, linked below.
Obesity || Food Security || Diabetes || Iron || Micronutrients
The Science Media Centre also contacted a number of leading experts in nutrition and public health for their comments on the survey.
Their responses are available below. Feel free to use these comments in your stories. To speak to an expert please contact the SMC (04 499 5476; smc@sciencemediacentre.co.nz).
Prof Winsome Parnell, an Associate Professor in the Department of Human Nutrition, University of Otago, was the Nutrition Director for the survey. She provided the following comments on the survey results:
“The public should be re-assured that the Ministry of Health funded this survey. This research will provide a great deal of baseline data that will be picked up by nutritionists and other academics. It will inform future policy making and scientific research.
“We didn’t actually do this nutrition survey specifically to document obesity — because that is done well in health surveys — and it merely underpins concerns that we have had for a considerable time.
“In terms of obesity, the different ethnic groups experience overweight and obesity differently — that’s a much bigger influence than the level of deprivation. Though the index of deprivation does show that women, more so than men in the most deprived areas, are more likely to experience overweight and obesity.
“The data has enable us to look clearly at what is happening across age groups. If there is any area of concern, it is the (energy) intakes of younger people.
“We have not done statistical comparisons between ethnic groups. The Ministry (of Health) plans to do those in the future. The socio-economic distribution of population is different for different ethnic groups. Initial analyses have not untangled those two to show whether one is more or less important than the other, but future analyses will do that. It is clear that obesity is higher among the Maori and Pacific groups, than the New Zealand European and other ethnic groups (NZEO). But if you look at change over time, it is the NZEO where you can see a marked increase in rates of obesity.
“The survey marked an imbalance related to energy intake but did not measure energy expenditure or show whether intake or physical activity is more important.
“There were some things I hadn’t expected to see, such as the lower vitamin A levels.
“We had suspected that the iodine status was low, but this was the first time that we had a look at the whole population, and as we found with (earlier studies of) the children, it was not ideal. But some things have been put in place and this type of data will help us check that adding iodised salt to bread is effective.
“It was interesting that older people were more likely to routinely take nutritional supplements. This may be because they are prescribed supplements, and older people take more oils promoted as good for joint health.This was the first survey where we have noticed such a high intake of those, and we acknowledge that they are highly promoted.
“Young people are more likely to use supplements episodically. They try multivitamins, often because they say it”s better than worrying about their diet. There is an attitude out there that nutritional deficiencies can be made up by supplements or pills. In reality, spending the money on healthy food would be better, but it’s easier to take a pill.
“I probably had inklings about what was happening with household food security, bodyweight status and diabetes. Three-quarters of the population said they were fully food secure in 1997, but only about 60 percent say that this time, while a greater proportion of people report lower food security. Among people in the most deprived circumstances, up to 20 percent reported low food security, which is of concern.
“The actual calcium intake had not declined since 1997. But there is a very high official recommended level for Australia and New Zealand at present. If you accept that recommended level is wise, then we’re nearly all having an inadequate intact. However, some experts say our recommended level is relatively high, and this survey points to the need for further research whether our bone density levels are healthy.”
Professor Jim Mann, Professor of Human Nutrition and Medicine at University of Otago and consultant on the survery, comments:
“The obesity figures are alarming, but not surprising: we are high up in the ranks of the global pandemic of obesity. It reminds us that we have got a terrible problem … clearly, we need to be doing something about it. Obesity is particularly common in people who are socioeconomically deprived.
“Energy intakes are difficult to measure accurately, but we must be eating more than we are putting out in activity. We’ve got to put out more, and maybe eat less of the wrong kind of foods. What we are talking about is excessive intake of energy-dense foods, those high in fat and high in sugar. It looks as though consumption of saturated fat is coming down. That’s good news, though lower cholesterol levels could also be because there are vast numbers of people on statin drugs.
“The number of people with diabetes are almost certainly underestimated. While things are being done, one of the big concerns of people like myself is we don’t really have an overarching strategy for dealing with the obesity/diabetes epidemic. Rising obesity prevalence has longer-term implications for the incidence of cardiovascular disease — it may start rising again — and some cancers.
“We need an overarching strategy to deal with obesity and the prevention of diabetes, and prevention of all the other long-term consequences. We used to have a strategy — the Healthy Eating-Healthy Action (HEHA) — but it wasn’t in place long enough to find out if it was working. Parts of it are still around, but fruit in low-decile schools was only a tiny start towards creating an environment to encourage healthy food choices and physical activity choices.
“That’s what an overarching strategy does — and that’s what we haven’t got at the moment”.
Professor Elaine Rush, Professor of Nutrition, Faculty of Health and Environmental Science, Auckland University of Technology, comments:
“The report is comprehensive and detailed and is, as the authors point, out useful for the development of policy and for monitoring. Much has changed in 11 years. For adults the relatively large decrease from 1997 to 2008 in food security and the increase in body size for height is a huge concern for all New Zealanders.
“These measures are indicators that, as a country, we have a dire and worsening problem. In New Zealand, since 1997, the gap between the rich and poor has widened, the cost of food has increased by more than 50%, unemployment has increased particularly for youth and the number of children living in poverty has remained high. In the next 15 years the number of New Zealanders aged over 65 years will exceed the number of children age 0-14 years. What does this mean for our future as a country and for our children and their children?
“This survey was not of children, it was of their parents, whanau and communities. If adults are not able to eat well then how can we expect our children to be different? Overweight and obese mothers have bigger babies who are more likely to become overweight adults but more importantly have more chronic disease. But it is not just how much you weigh but how functionally fit you are.
“There are differences in body composition by ethnicity and risk profiles. Indian people have more risk of diabetes than Maori, Pacific, Chinese and European at a much smaller body size. It is unfortunate that European are not a stand alone group like Maori and Pacific, other ethnicities are included with European so the statistics for the (still but decreasing) majority population are not clear. The increasingly diverse and multiethnic profile of New Zealand adds complexity to the interpretation of these findings and actions that should be taken.
“The biggest whammy is for people living in more deprived areas. They are more likely to be overweight or obese, not meeting recommended micronutrient intakes such as iron, vitamin A and calcium. Bread continues to be the major contributor of energy, protein, and carbohydrate to the New Zealand diet, In comparison to white bread, light or heavy whole grain bread was chosen by 60% of the population, but almost 50% of young adults compared to 25% of older people reported eating white bread. The most socioeconomically deprived 20% were twice as likely to consume white bread compared to the most well off 20% (20% vs 40%).
“The evidence is clear, in 2008 New Zealanders were not well nourished, many did not have enough money to buy nutritionally adequate and safe foods and were not healthy. Since then the economic recession and the ever-increasing cost of food mean that we are unlikely to be improving. More importantly our present children and those still to be conceived are not likely to have an optimal start to life continuing the cycle. A whole of New Zealand response is required because it is not a personal choice or responsibility- particularly for children. We produce enough good food to feed everyone well – why the gap between the farm and the mouth?”
Delvina Gorton, National Nutrition Advisor, NZ Heart Foundation, comments:
“Nutrition surveys happen every ten years, and they are our chance to see how New Zealanders are doing with what they eat and their health. One of the really concerning issues in the survey is the number of households in New Zealand who are struggling to feed their families.
“We have all felt the impact of rising prices for necessities like food and fuel over the past few years. For people who are living on strict budgets, these increases are obviously felt more strongly as income hasn’t kept up. Food, although a necessity, is not a fixed amount in the budget, so often less food is bought in order to pay other bills. When one in every fourteen households are having to rely on other people or on food banks to feed themselves and their family, we have a big problem.
“Lack of food security is strongly related to income – how much money people have available to put food on the table. So it is usually a much bigger problem for those on a low income. This includes proportionately more M?ori and Pacific families, who on average have lower incomes.
“Kiwis are generally caring people who want everyone to have the basics they need to survive – including food on the table. But food security is not just a question of fairness, lack of it is linked with having a less healthy diet, nutrient deficiencies, higher rates of disease and obesity, stress and depression, poor academic development, and behavioural and psychosocial issues in kids – so it has major implications.
“There’s no quick fix. There are a lot of initiatives that can help, such as fruit in schools, community gardens, or community fruit and vegetable markets. But to really fix the problem incomes need to increase and healthy food become more affordable. This requires cooperation between government departments, industry and communities to work together on a wide range of issues. An example of one promising strategy is an electronic discount card that could be targeted to healthy food for hard-up families.”
Bronwen King, Public Health Nutritionist, Partnership Health Canterbury, comments:
“While I agree that lack of physical activity could be a cause for an increases in BMI, I believe it is just a drop in the ocean compared to the true cause of weight gain. Weight gain is far more complex than simply energy in versus energy out. There are many factors that influence our physiology and propensity to gain and store fat.
“The type of kilojoules consumed can influence weight gain. Kilojoules that come from sugar and other refined carbohydrates enter the blood stream quickly, cause fast sharp rises in blood glucose which in turn generates a large insulin response. Since insulin promotes fat storage, people consuming a highly refined diet are likely to be more prone insulin resistance, type 2 diabetes and to storing fat and gaining weight.
“Other factors that impact on a person’s ability and propensity to gain weight include hormones, stress levels, lack of sleep, the speed at which we eat, tv watching and even our work practices to name but a few. Modern day living affects our physiology in many complex ways – we are discovering more of these every day. We are just realising for example, the impact that extended bouts of sitting have on our health and weight – and that even if you do an hour walking or in the gym it does not compensate for this. Since modern day living involves a lot of sitting, this has to be part of the reason we are gaining weight.
“I am not totally convinced that there is a drop in overall kilojoule intake either – food recall is notoriously inadequate with under reporting the norm. Brian Wansink, a professor at Cornel University, USA, in his book “Mindless Eating” talks about this as the mindless margin, ie the difference between what we think we eat and what we actually eat and he has demonstrated through experiments, that the more people eat, the harder it is to recall it all.
“Food marketers and manufacturers are masters in the art of making us eat more than we think – simple things like package sizing all influence our kilojoule intake and package and portion size is increasing. People will finish the package and state “I only had a packet of…… regardless of the size and regardless of the fact that one package may in fact be 2 or 3 servings! The same with café style giant muffins (that are now the norm but are actually the equivalent of 3 of the muffins that were the norm 20 years ago) Big portions are the new norm and our health and weight are suffering. ”
Prof Rod Jackson, Professor of Clinical Epidemiology & Biostatistics,University of Auckland, comments:
“On the interpretation of the observation that self-reported energy intake has fallen while obesity has increased – I would suggest that this is due primarily to an under-reporting of energy intake rather than a reduction in activity levels, for 2 reasons. Firstly, self-reported food intake is notoriously unreliable and people under-report consumption. Moreover given the huge focus on over-eating and obesity in recent years, it is very likely that there will be greater under-reporting now than when the last Nutrition survey was done. Secondly, the international literature consistently demonstrates that increased food intake, rather than decreased activity, is the main determinant of increased fatness.”
Further findings of the 2008-2009 Adult Nutrition Survey (NZANS)
In the most recent survey, men reported a mean daily energy intake of 10.7 megajoules (MJ) — more than 2479 calories in older-style measurements — compared to the 12 MJ recorded in 1997. Women also dropped, from 8MJ to 7.6MJ — though this was not statistically significant.
“This reported decrease in energy intake is inconsistent with trends in body size,” the researchers said in the survey report released on the Ministry of Health website today.
Over the same period, the prevalence of obesity soared, said Ministry of Health and Otago University researchers who surveyed 4721 people.
“After adjustment for age and ethnic group, the prevalence of obesity in 2008/09 compared to 1997 was 1.5 times higher for males and 1.3 times higher for females,” the researchers said in the 330 page report.
In a report on the latest research, A Focus on Nutrition, the height and weight of people surveyed was used to calculate body mass index (BMI). The heights measure remained the same, but the survey showed the mean BMI rose with increasing levels of “neighbourhood deprivation”, after researchers adjusted for age, gender and ethnic group.
World Health Organisation (WHO) cut-off points said anybody with a BMI level of more than 30 was obese, and the highest mean BMI of 32.3 was notched up by Maori women aged 51 or older, who weighed up to 85.1kg. They were just behind Maori men aged 31-50 years, who weighed up to 105kg and had a mean BMI of 32.2. In the total population, both men and women aged 31-50 hit the top BMI of 28.8, with the men weighing up to 88.7kg and women up to 75.4kg.
“The increase in mean body weight, BMI and obesity prevalence suggests that energy balance is unbalanced, with energy ‘in’ exceeding energy ‘out’,” the researchers said. The drop in the reported mean daily energy intake over the 12 years included a slight fall in the contribution fat made to energy in the diet for men — with an insignificant drop for women — and both groups took less energy from saturated fat and more from monounsaturated fats. Their drop in total fat consumption was offset by an increased proportion of energy coming from protein.
Total blood cholesterol levels — an important risk factor for cardiovascular diseases — dropped in both men and women, but the researchers said that part of this could have been due to people eating less saturated fat, but increased prescribing of lipid-lowering drugs was also likely to have played a role
 Nutritionists say that there has been a big jump in recent years in the proportion of households classed as having low “food security” .
Nutritionists say that there has been a big jump in recent years in the proportion of households classed as having low “food security” .
Food security is access to adequate, safe, affordable and acceptable foods — but 7.3 percent of households in a big survey by the Ministry of Health and Otago University researchers were classified as having low food security, difficulty in acquiring nutritionally-adequate foods. “Since 1997, there has been … an increase in the prevalence of low food security,” the researchers said in a report, A Focus on Nutrition, released on the Health Ministry website. Nearly 60 percent of the households questioned were classified as being fully or almost “food secure” — in 1997 78.5 percent of men and 73 percent of women fitted this category.
Another 33 percent were classified as being moderately food secure — a lift of 10 percentage points.
But over the 12 years from 1997, the proportion of households with low food security surged from 1.6 percent for men to 5.6 percent, and from 3.8 percent for women to 8.8 percent.
Earlier this year, a separate Otago University study linked growing food insecurity to elevated levels of psychological distress amongst thousands of adults.
Food insecurity or the lack of access to safe, nutritious, affordable food, not only affected nutrition and physical health, but also the mental health of New Zealanders, that study said.
It said that 16 percent of nearly 19,000 adults from the Survey of Families, Income and Employment 2004/05 was classified as “food insecure” because those people used food banks or grants, had to buy cheaper food to pay for other things, or often went without fresh fruit and vegetables.
 Nearly 7 percent of New Zealanders have diabetes, and a new nutrition survey shows that over quarter of them don’t yet know it.
Nearly 7 percent of New Zealanders have diabetes, and a new nutrition survey shows that over quarter of them don’t yet know it.
The 2008/09 Adult Nutrition Survey (NZANS) canvassed 4721 New Zealanders aged 15 years and over. Blood samples tested for glycated haemoglobin (HbA1c) showed 6.9 percent of them had diabetes, with men at 8.4 percent and women 5.6 percent. But 2 percent of the undiagnosed population had not been told this by a doctor, even though their HbA1c levels were 6.5 percent or greater. Researchers noted the actual proportion of undiagnosed diabetics might actually be higher.
Less that half (48.5 percent) of the people who knew they had diabetes had good control of the illness, according to the survey, which was released on September 15 — the same day that the Government announced it was axing a programe that provided free annual medical checks for patients with diabetes. Separately to the nutrition survey, which was conducted by the Ministry of Health and Otago University researchers, the ministry’s national clinical director for diabetes, Brandon Orr-Walker, said the Diabetes Get Checked Programme provided no better results for those on it than for patients on standard health care.
Diabetes is a metabolic condition which results in raised blood glucose levels, and it causes a lot of deaths through illnesses such as cardiovascular disease, blindness, kidney disease and vascular problems that damage nerves to the point that amputation of feet is necessary.
The mean HbA1c level in the survey was 5.57 percent, but there were major variations between different population groups. In the total population, the highest levels were recorded in people over 71 years, with men at 6.01 percent and women at 5.52 percent, and there was a consistent trend upwards from 19 years through to people over 71.
Among people who had been diagnosed by a doctor, the highest mean levels seen among pakeha (New Zealand European and others) older than 51 years were 13.3 (men) and 7.1 (women). Among diagnosed Maori of the same age, the levels hit 20.9 (men) and 23.8 (women). The median levels for diagnosed Pacific Islanders in the same age were 22.7 (men) and 21.4 (women).
Iron deficiency in New Zealand’s women more than doubled over the 12 years to 2009, and an increasing proportion of other women have low iron levels, nutritionists say.
 Iron is required for the production of a number of proteins in the body, including haemoglobin which is needed to transport oxygen in the blood and make it available to tissues throughout the body. There are three stages of iron deficiency. In the first stage, body iron stores start to become depleted. In the second stage, levels of circulating iron start to fall, although blood haemoglobin concentrations are maintained. In the final stage, body iron stores are severely depleted and iron deficiency anaemia occurs. Iron-deficiency anaemia is associated with decreased work capacity, fatigue, and some specific cognitive learning effects.
Iron is required for the production of a number of proteins in the body, including haemoglobin which is needed to transport oxygen in the blood and make it available to tissues throughout the body. There are three stages of iron deficiency. In the first stage, body iron stores start to become depleted. In the second stage, levels of circulating iron start to fall, although blood haemoglobin concentrations are maintained. In the final stage, body iron stores are severely depleted and iron deficiency anaemia occurs. Iron-deficiency anaemia is associated with decreased work capacity, fatigue, and some specific cognitive learning effects.
Iron deficiency is a particular problem among women, with this new 2008-2009 Adult Nutrition Survey (NZANS) released on the Ministry of Health website (on September 15 2011) showing that around one in three girls aged 15 to 18 have an inadequate intake of iron. Inadequate intakes were found among 15.4 percent of women aged 31 to 50 years.
An iron deficiency was found in 2.9 percent of women in a national nutrition survey in 1997, but, 12 years later, this had risen to 7.2 percent. After adjusting for age and ethnicity, there was an increase in the prevalence of low iron stores in women.
Overall, 4.2 percent of the 4721 people surveyed were iron deficient, and 2 percentof the participants had iron deficiency anaemia. Among women, iron deficiency affected 7.2 percent and iron deficiency anaemia affected 3.5 percent. High levels of iron deficiency were found in girls aged 15 to 18 years: prevalence of iron deficiency was 10.6 percent and iron deficiency anaemia 4.9 percent. But the highest prevalence was among women aged 31 to 50 years (12.1 percent prevalence of iron deficiency, and 6 percent prevalence of iron deficiency anaemia).
The survey showed breads provided 12 percent of dietary iron, but other big sources were breakfast cereals (10 percent) vegetables (8 percent), grains, pasta, beef, and veal (each 7 percent) potato, kumara and taro (each 6 percent). Iron in meat, fish and poultry — known as “haem” iron — is better absorbed by the body than the non-haem iron found in vegetable and cereal foods. However, the absorption of non-haem iron can be boosted by eating meat and foods containing vitamin C at the same time The iron requirements of vegetarians are about 80 percent higher than for non-vegetarians.
Compared with 1997, the latest survey showed both men and women consumed higher levels of vitamin B6 and the mineral selenium, and women got more vitamin E. But both men and women missed out on several key nutrients, including zinc and potassium, and vitamin A. Men also ate less sucrose, vitamin C and iron, and figures adjusted for age and ethnicity, showed a drop in calcium for men, and thiamin for women, and riboflavin for both groups. The percentage of adults eating a recommended three servings of vegetable each day did not change, but more men and women began eating the two servings of fruit also recommended by health officials.
Calcium
Nearly 60 percent of New Zealanders over the age of 15 years get too little calcium in their diet, and the shortfall is much worse for teenage girls, a new nutrition survey reports.
 Over 95 percent of Maori girls aged under 19 were missing out, and over 87 percent of all girls fail to get recommended intakes — an important issue because peak bone mass was developed during young adulthood. Estimated average daily requirements Ministry of Health and Otago University researchers used to make their calculations said the teenagers under 19 should be getting 1050mg a day.
Over 95 percent of Maori girls aged under 19 were missing out, and over 87 percent of all girls fail to get recommended intakes — an important issue because peak bone mass was developed during young adulthood. Estimated average daily requirements Ministry of Health and Otago University researchers used to make their calculations said the teenagers under 19 should be getting 1050mg a day.
Reserves of calcium in the skeleton can be important later in life as bone density declines. Calcium is also important to muscle and nerve functioning, blood clotting and blood pressure. But researchers who compiled the 2008-2009 Adult Nutrition Survey (NZANS) — released on the MoH website on September 15 — said the adequacy of calcium intake was “difficult to interpret” and global experts worldwide didn’t agree on the best levels. The latest figures were in line with those in the 1997 National Nutrition Survey held a dozen years earlier.
Recommended dietary levels were high, but calcium intake was only one of many factors — such as vitamin D status, physical activity levels and habitual levels of intake– that affected bone health., the researchers said. The median usual daily intake of calcium was 919mg for men and 745mg for women. Maori ate less (863mg for men, 711mg for women) and Pacific Islanders lagged even further (men 693mg and women 604mg).
Milk and some other dairy products such as yoghurt and cheese were important sources of calcium, and non-dairy sources of calcium included tinned fish with bones, green leafy vegetables, nuts and seeds, and fortified soy and rice “milk”.
Zinc
 Nearly a quarter (24.7 percent) of New Zealanders aged 15 years and over were not getting enough of the trace element zinc in their diet, with 39.1 percent of men and 11.2 percent of women missing out. The median usual daily intake of zinc was 12.9mg for men and 9mg for women, and even lower for older people.These intakes were down those seen in the 1997 survey.
Nearly a quarter (24.7 percent) of New Zealanders aged 15 years and over were not getting enough of the trace element zinc in their diet, with 39.1 percent of men and 11.2 percent of women missing out. The median usual daily intake of zinc was 12.9mg for men and 9mg for women, and even lower for older people.These intakes were down those seen in the 1997 survey.
Zinc is important in major metabolic pathways, including protein and nucleic acid synthesis, the action of insulin and in growth, immune function, wound healing, sperm generation and foetal development.
Rich sources of zinc include oysters, red meat, lamb’s liver and cheese, and someof the biggest contributers to the survey participants were beef and veal, bread, grains and pasta, which each contributed about 10 percent of their intake.
Selenium
Over half of New Zealand women and about a third of men are not getting enough selenium — a trace mineral deficient in the nation’s soils. Though intakes in the new survey were higher than in 1997, they were still inadequate for 45 percent of the population aged 15 years and older: about 31.5 percent of men and 58.2 percent of women. Over 70 percent of teenage girls under 19 did not get enough selenium.
 Fruit, vegetables and grains grown in New Zealand tend to have lower selenium levels than plant foods from countries with higher levels in their soils.
Fruit, vegetables and grains grown in New Zealand tend to have lower selenium levels than plant foods from countries with higher levels in their soils.
Bread was the largest single contributor of selenium to the nation’s diet (15 percent), but the survey did not allow for regional differences, even though in the North Island, bread is mainly made imported wheat, which has a higher selenium content than New Zealand flours. Seafood (12 percent) and poultry (10 percent) were also important sources of selenium, which is f important to antioxidant defences, thyroid metabolism, and immune and reproductive functioning.
The median usual daily selenium intake was 67 micrograms (mcg) — millionths of a gram — for men and 47.1 mcg for women.