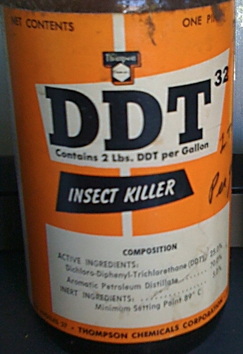
UK SMC: An increased risk for Alzheimer disease appears to be associated with elevated blood levels of a byproduct of the pesticide DDT, which was banned in New Zealand in 1989 but is still used for agriculture in other countries. An accompanying editorial and a UK SMC round up and both warn this research should be considered preliminary.
 Professor David Coggon, Professor of Occupational and Environmental Medicine, University of Southampton, comments:
Professor David Coggon, Professor of Occupational and Environmental Medicine, University of Southampton, comments:
“From an epidemiological perspective this paper is rather unsatisfactory, in that we are told rather little about how the cases and controls were recruited. This makes it difficult to assess whether the exposures of controls are likely to have been representative of the population at risk of being included in the study as cases (a key requirement in case-control studies).
“A further concern is the possibility that loss of weight as a consequence of Alzheimer’s disease could have led to changes in levels of DDE in the cases.
“The findings should be a stimulus to further research using more rigorous epidemiological methods, but of themselves, they do not provide strong evidence of a hazard. As DDT has been banned in the UK for many years, there is no scope for additional regulatory controls on a precautionary basis.”
Professor Kevin McConway, Professor of Applied Statistics, The Open University, comments:
“This paper absolutely has to be read alongside the accompanying editorial by Steven DeKosky and Sam Gandy, in the same issue of the journal, which points out the main problems in its interpretation. The sample sizes were pretty small, and DeKosky and Gandy point out that the overall difference between DDE levels in people with Alzheimer’s and the controls was entirely due to the data from Texas – there was no such difference at the other study site (Emory University in Atlanta, Georgia). This demonstrates the difficulty in a study of this nature, of sorting out what causes what. Maybe the lack of association between DDE and dementia in Georgia was a statistical fluke – but maybe the association in Texas was a statistical fluke instead. Maybe many of the Texans with high levels of DDE had worked in some particular industry where their exposure to DDT was high, and maybe it was a different feature of their work that increased their chances of developing Alzheimer’s disease, and nothing to do with DDT at all. We just can’t sort out these questions of what causes what from this study. I’m with DeKosky and Gandy when they say, “in our opinion, the Richardson et al. report should be noted but, for now, these conclusions should be considered as preliminary until there is independent confirmation in other populations.” So yes, let’s keep looking, but let’s not get too anxious.”
Information from the UK Food Standards Agency:
DDT was banned in the UK in 1986. Signatories of the Stockholm Convention on Persistent Organic Pollutants, a global treaty, agreed to ban agricultural uses of DDT in the 2000s by which time most countries had already banned it. DDT is therefore extremely unlikely to be used on any food products imported to the UK and will not be used on products grown in the UK.
DDE is formed when DDT breaks down. DDE has been found at very low levels in fatty meats, full-fat dairy products and oily fish due to historical use of DDT. Levels of DDE have been falling over the last 30 years.
Levels of DDT in the body fat of people in the UK have been decreasing since the 1960s, and levels of DDE have been falling since the late 1970s.
This American study does not give conclusive evidence that DDT or DDE are risk factors for Alzheimer’s disease. Further studies would be needed to explore this association further.
Prof Tony Dayan, Emeritus Professor of Toxicology, University of London, comments:
“As the accompanying editorial in JAMA Neurology notes there is reasonable evidence that unidentified, non-genetic factors appear to be very important in the causation of Alzheimer’s Disease (AD). That must always suggest ‘environmental’ factors that might include diet, life-style, pollutants and prior exposure to chemicals of any sort.
“Richardson and his colleagues have now provided evidence that the level of a long-lived metabolite of DDT in blood and brain is statistically associated with the occurrence of typical AD in a group of patients in Texas. Their statistical handling of the data is sophisticated and they have taken a case-control study about as far as it can go. As the accompanying Editorial points out many uncertainties remain in the claimed association and its relevance to the cause of the disease remains quite uncertain.
“Their work points to the value of other surveys that could be done using existing material, e.g. the vast NAHNES cohort collected by the NIH in America, which has previously been used to explore whether there was any link between pesticide exposure and cancer of the breast in women, etc. Attention might also be given to the incidence of AD in parts of the world where DDT was once widely used to protect populations against malaria and other fatal insect borne diseases, e.g. Sri Lanka, the Gambia and other parts of Africa and SE Asia.
“But hope of finding pesticide exposure, or more specifically DDT exposure, as an important causal factor in AD should not be too high. The disease has been well known since well before DDT was even first synthesised and certainly before it was ever used as an insecticide. Experience of DDT over decades in tests in animals and humans has not suggested any actions relevant to the signature lesions of AD. Also, the brief in vitro experiment mentioned by Richardson et al reflects circumstances and exposure remote from human or veterinary experience of exposure to DDT. Indeed, since DDT was once widely used to protect farm animals it is reasonable to ask whether there was any evidence suggesting AD-like effects or changes in them?
“An association between many different pesticides and several neurological diseases has often been mooted, as the Editorial notes, but it has not yet proved possible to link such exposures with the disease in any consistent or strong way nor has any realistic disease-causing mechanism yet been proposed.
“The new work is useful reminder that many diseases may have environmental associations and that the environment is often too complex for simple one-factor effects to be demonstrated and then proven.”
Prof Alan Boobis, Professor of Biochemical Pharmacology, Imperial College London, comments:
“The accompanying editorial is well balanced and highlights many of the caveats in this study. I fully agree with the key conclusions of the editorial, that the report should be noted but the conclusions should be considered as preliminary, and need independent confirmation in other populations.
“In most countries (including the UK), DDT is no longer used and in those countries where use is permitted, its use is very restricted. The authors of the paper have looked for associations between DDT/DDE levels and Alzheimer’s Disease occurrence, but from the evidence they present we still don’t know whether DDT/DDE might be associated with Alzheimer’s Disease through the much higher exposures that occurred several decades ago, or through the lower levels of exposure occurring now from residual environmental levels. This distinction is important because some confounding factors have not been accounted for in this study, for example co-exposures in the past, many of which would no longer be detectable in biological samples.”
Prof Carol Brayne, Professor of Public Health Medicine, University of Cambridge, comments:
“This is a case control study, which are notoriously subject to the influence of recruitment methods; for example, in the past smoking has been thought to be protective for dementia from studies using this design. It is very difficult to interpret the results usually, and particularly in dementia, and I would be very very cautious indeed about over-interpreting the results at this stage without confirmation from research based on stronger designs. I would have been very interested to see the DDE results in relation to educational level, which might have introduced residual confounding (the controls have higher levels of education and most of the cases have the same level of DDE so it is driven by a minority with higher measures – see Figure 1). I would have been interested in what characterises a high exposure irrespective of caseness (i.e. distribution within an unselected population and examining broader characteristics). However, this is clearly a very interesting result that should be followed up in existing longitudinal studies which have measurement available in a prospective manner.”
[DDE is the metabolite of DDT.]
* ‘Elevated serum pesticide levels and risk for Alzheimer disease’ by Jason R. Richardson et al. was published in JAMA Neurology at 21:00 UK time on Monday 27 January 2014.