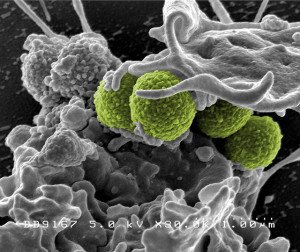
The jury is still out on the effectiveness of meticillin-resistant Staphylococcus aureus (MRSA) superbug control policies in hospitals, according to leading infectious disease experts in a Viewpoint published in The Lancet.
In particular, screening and isolating infected patients-which have long been regarded as the gold standard MRSA prevention strategy and are required by law in some countries-have poor evidence for their effectiveness, say the authors. The authors note that the research supports hand washing and antibacterial baths as effective tools for combating the spread antibiotic resistant microbes such as MRSA.
“With the tide of MRSA receding and improved treatment options for the infection, a window of opportunity now exists to reassess whether masks, gowns, gloves, single rooms, and cohort nursing add anything to hand hygiene and decolonisation, and to find a proper balance between effectiveness and harm,” conclude the authors.
“Recommendations and guidelines should clearly state the uncertainties in this field, and legal mandates dictating specific infection-control practices for MRSA should be abandoned. We owe our patients no less.”
Our colleagues at the AusSMC collected the following expert commentary. Feel free to use these quotes in your reporting. If you would like to contact a New Zealand expert, please contact the SMC (04 499 5476; smc@sciencemediacentre.co.nz).
Professor Peter Collignon, Infectious Diseases Physician and Microbiologist at the Canberra Hospital, Associate Executive Director of ACT Pathology and Professor, Medical at Australian National University, comments:
“These authors conclude that hand hygiene and decolonisation are effective in controlling MRSA, with which we would all agree.
“They wonder if masks, gowns, gloves, single rooms, and cohort nursing add anything more and we need to find a proper balance between effectiveness and harm.
“It makes sense to do good studies to answer these questions.
“Certain countries, however, that do all of this – such as The Netherlands and Denmark – have the lowest rates of MRSA spread in healthcare facilities as does WA in Australia.
“So, we need to make sure that studies clearly show that we will not do harm by stopping some or all of these isolation methods.”