Japanese researchers have successfully produced functional mouse eggs entirely in cell culture using stem cells.
Their study, published today in Nature, resulted in healthy and fertile mouse pups. The researchers say being able to grow viable mouse eggs in the lab will provide clues to aid the development of similar systems in other species.
More information is available on scimex.org.
The SMC collected the following expert commentary. Feel free to use these quotes in your reporting.
Associate Professor Alan Davidson, Department of Molecular Medicine and Pathology, University of Auckland, comments:
“This work solved a major hurdle in the field — how to convert pluripotent stem cells, capable of forming any cell in the body, into female gametes (eggs) that could be fertilised.”
Dr Teresa Holm, research fellow, Department of Molecular Medicine and Pathology, University of Auckland, comments:
“The study used mouse cells but if it can be translated to humans, and shown to be safe, it could theoretically provide a treatment for female infertility in the future. In the meantime, this approach provides a valuable new tool to study the normal biology of egg formation and how this process goes awry in certain diseases or birth defects.”
AProf Davidson and Dr Holm work in human pluripotent stem cell research at the University of Auckland.
Our colleagues at the UK Science Media Centre gathered the following comment.
Prof Azim Surani, Director of Germline and Epigenomics Research, The Gurdon Institute, University of Cambridge, comments:
“This study represents a major accomplishment; it is very impressive indeed. Hayashi had previously taken major steps towards achieving full development of mouse eggs in culture, and he has accomplished that objective in this new paper.
“The work is robust and in my view will be reproduced by other labs. Now we need additional data and observations, particularly on term embryos to see how many develop normally and what happened to those that did not. Do we anticipate or observe any developmental abnormalities?
“Ethically, this issue has yet to be discussed fully by the scientists and society. These discussions have occurred in the past, and are continuing within the regulatory bodies, certainly in the UK. This indeed is the right time to start a debate and involve the wider public in these discussions, long before and in case the procedure becomes feasible in humans.
“To replicate this work in humans poses further challenges, and it is futile to speculate when this will become possible. There are some key differences that have become evident between mouse and humans germ lines, which we described in our publications last year, which have to be taken into account. Second, it is possible that the procedure may require a considerably long culture period, which while not insurmountable, adds to the difficulties. For example, environmental factors during culture could cause aberrant epigenetic modifications (modifications that do not affect the DNA sequence but are potentially heritable and can affect gene expression in the progeny), which could affect development of synthetic eggs. Third, the mouse procedure requires co-culture of germ cells with fetal gonadal cells for their maturation into oocytes. This step might be difficult if it requires human fetal gonadal cells. We may need to find alternatives, for example replacement with additional factors or finding alternative cells for co-culture.
“We in my lab are working on the initial stages of developing human primordial germ cells currently. We have much to learn about the human germ cell biology in order to ask questions, such as the mechanism of the unique epigenetic program of the germline that is essential for producing normal gametes. Other related research areas include mitochondrial biology, infertility and germ cell tutors. Advances in these areas could be widely applicable towards understanding age related diseases and in regenerative medicine.”
Prof Martin Johnson, Professor of Reproductive Sciences, University of Cambridge, comments:
“This paper reports the generation of fertile mice from eggs derived entirely in-vitro from stem cells – both embryonic and induced stem cells – and is a remarkable achievement, involving good quality research, conservatively interpreted, in which the conclusions are supported by reliable data.
“The data are primarily of interest to scientists, although potentially of clinical interest to those patients who lack eggs of their own.
“However, there are major limitations for the application of this technology to the clinic, acknowledged in the paper, and including: 1. a requirement to use granulosa cells during the in-vitro maturation phase; 2. the fact that the gene expression patterns in many or most of the fully matured in-vitro derived eggs differs significantly from that in control eggs; 3. the fact that chromosomal abnormalities are more common in the in-vitro derived eggs; and 4. that, probably as a result of 2 and 3, only a small number of embryos formed from in-vitro derived eggs developed into ‘normal’ young.
“For these reasons alone, the application of this technology to the human is years away.”
Prof Richard Anderson, Honorary Consultant in Obstetrics and Gynaecology & Professor of Clinical Reproductive Science, MRC Centre for Reproductive Health at the University of Edinburgh, comments:
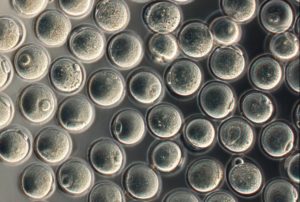
“This new report from Professor Hayashi and colleagues provides a substantial advance in our understanding of how artificial eggs might be made. They start from embryonic stem cells, and make an artificial ovary in which the stem cells turn into immature oocytes, and then mature within follicles just as they would normally. They were able to fertilise these eggs using IVF, and generate healthy fertile pups. This is the first report of anyone being able to develop fully mature and fertilisable eggs in a laboratory setting right through from the earliest stages of oocyte development. Importantly, they carried out a number of safety checks along the way, which as might be expected showed that these eggs do not develop quite as well as normal eggs, but these findings will lead to new avenues to explore the genes and pathways that control normal egg development.
“Although we are a long way from making artificial eggs for women at the moment, this study also provides us with a basis for experimental models to explore how eggs develop from other species, including in women. This is extremely challenging at the moment due to the difficulties of getting eggs to study, so being able to develop them in the laboratory would greatly improve this.
“One day this approach might be useful for women who have lost their fertility at an early age, as well as for improvements in more conventional infertility treatments. But the very careful analyses in this paper show the complexity of the process and how it is a long way from being optimised.”
Dr Dusko Ilic, Reader in Stem Cell Science, King’s College London, comments:
“Scientists from Japan were able to reconstitute the full process of making an egg in a dish. Cells from a mouse tail were reprogrammed into embryonic-like induced pluripotent stem cells (iPSC) lines, which were then used to generate in the lab fully potent mature eggs capable of producing offspring.
“To do that, at one stage the scientists co-cultured iPSC-derived primordial germ cell-like cells with female gonadal somatic cells from 12.5-day old mouse embryos. The next step would be to circumvent the use of embryonic tissue and reconstitute the entire process in a dish from iPSC. However, it may take years before we reach this point.
“If (when) this happens, developing similar culture systems in other species should be only a matter of technicality and with such technology we might be able to rewind the process of mammalian extinction.”
Prof Robin Lovell-Badge, Group Leader, The Francis Crick Institute, comments:
“This is an interesting piece of work, but like the topic – how to make eggs in vitro – it should be considered as a beginning, albeit a very promising one, and not an end. This is the first convincing evidence that it is possible to go all the way from pluripotent stem cells, via a primordial germ cell state, to functional oocytes entirely in vitro, which can then be fertilised and give rise to apparently healthy mice. The authors have carefully monitored progress through all the steps, ensuring that critical milestones are achieved by at least a proportion of the developing oocytes. And the methods they have used all make biological sense.
“It does seem to be a rather inefficient process, with many losses at each step of oocyte development, and notably with very few fertilized eggs giving rise to pups, but then so is oocyte development in vivo. Loss of germ cells occurs naturally in human ovary development with only about 30% surviving between 20 weeks and birth, and then only about 1 in 1000 of the primordial follicles at birth will mature to ovulation. This is not well understood, although it may be a quality control process to ensure that only the best survive. But having a way to observe germ cells in vitro as they become oocytes and then grow and mature will be important to allow research into the reasons why and how this happens.
“There is also a long way to go before these methods could be adapted and used in humans. Although the first step, notably deriving primordial germ cells (PGCs) from pluripotent stem cells in vitro has been achieved, there is no guarantee that the rest will work. Indeed, it will be of interest and perhaps of benefit in its own right to explore the similarities and differences between human and mouse oocyte development, of which we already know there are some. Moreover, there is the question of time. It usually takes longer than a decade to have fully grown oocytes in humans. Will it take this long to recapitulate the process in vitro, which would pose immense practical challenges, or will parts of the process speed up in vitro where the constraints that normally operate in vivo will be absent; such as the need for pituitary hormones to synchronise what goes on in the ovary with the rest of the body? Oocytes don’t usually begin to mature until puberty, but they may do so much sooner if the right conditions can be found in vitro.
“Clearly, if applied to humans, being able to get functional eggs via reprogramming skin cells to iPS cells, would have importance in overcoming female infertility, e.g. due to cancer treatment as a child, but it also opens up many other uses in research, in regenerative medicine, and potentially in avoiding genetic disease. But there are still many practical and ethical challenges to be resolved. One of these would be a source of fetal ovarian cell types, but as the authors suggest, it may also be possible to derive these from the same starting population of pluripotent stem cells.
“For some potential uses and ethical challenges, see: http://www.hinxtongroup.org/Consensus_HG08_FINAL.pdf Although this was published in 2008, it is still very pertinent and it recognised many of issues, which have been debated at length subsequently.”
Our colleagues at the Science Media Center in Germany gathered the following comment.
Professor James Adjaye, Director, Institute for Stem Cell Research and Regenerative Medicine, Heinrich Heine University Düsseldorf, comments:
“Over the years several groups including these authors generated egg-like structures (PGCLCs- primordial germ cells-like cells) which lacked maturity and could not be fertilized in vitro / in the dish. Primordial germ cells (PGCs) are the precursor cells which can either form sperm cells or oocytes.
“In the current study, the authors have shown perfection by optimizing their previous protocols by mixing the mouse tail fibroblast-derived iPSC or ESC derived PGCLCs with cells originating from the ovary (gonadal somatic cells) of mouse embryos. These gonadal somatic cells provide the necessary nutrients (growth factors, cytokines and hormones) needed to mature the PGCLCs. This seems to be the missing ingredient in all the other previous experiments which failed to produce mature eggs.
“Several groups have published human PGCLCs derived from iPS and ES cells. In these studies the authors obtained egg like structures that lacked maturity. Of course maturation might be possible if human PGCLCs are mixed with ovary (gonadal somatic cells) from human fetus. This however is not realistic on ethical grounds.
“Additionally, even if this was allowed, the final and ultimate test for fully functional human ‘eggs in a dish’ would be the fertilization using IVF, which is also ethically not allowed.
“I would say that fully mature and functional ‘eggs in a dish’ should be first produced in large animals- pigs, sheep and cows before attempting in humans.“
“It is all a matter of ethics! It would be interesting to allow deriving human ‘eggs in a dish’ but not to be fertilized. Such studies will be useful to enable increasing our meagre knowledge on human oogenesis.”
“There has been a lot of high profile, ground breaking publications recently which have turned out to be not entirely true or purely false (the acid bath iPSC paper for example). I believe this paper was delayed in the review process I would assume because the work had to be independently reproduced by other laboratories – my assumption.”