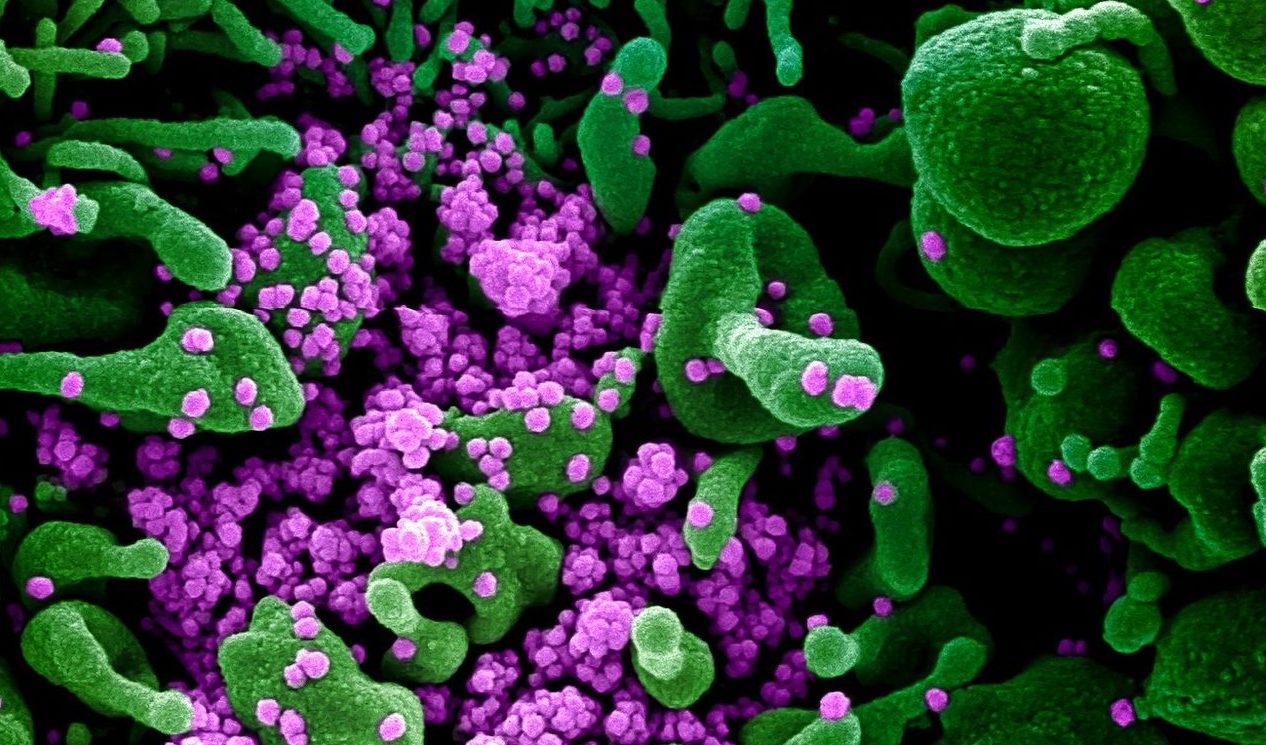
A pre-print study says there is a new, quickly spreading mutation of the SARS-CoV-2 virus.
The study – which has not been peer reviewed – also suggests the mutations could affect vaccine or treatment development.
The SMC asked experts to comment.
David Welch, Senior Lecturer, Centre of Computational Evolution and School of Computer Science, University of Auckland, comments:
“Mutations occur in all viruses. Most mutations do not change the epidemiology of the virus, that is, they don’t change things like how easily it is transmitted or how sick it makes people. Viruses that are the same, except for a few mutations, are often called different lineages. When a mutation arises that does materially change the viral epidemiology, we call it a new strain.
“No new strains of SARS-CoV-2 have yet been identified. But plenty of mutations have occurred and many different lineages are circulating. A recent article (that is not yet peer-reviewed) claims a new strain has arisen, based on a mutation (change from ‘G’ to an ‘A’) in a region coding for a protein important to the way the virus attaches to human cells. This is mainly based on observing that the proportion of viruses with this mutation has increased over time. They show that there is no difference in clinical outcomes for this lineage.
“Many factors could have caused the increased frequency of this mutation and it is very hard to separate them out. The biggest driver of the differing prevalence of viral lineages in different locations is chance. Most countries have seen multiple introductions (New Zealand, for example, had over 500). Chance dictates which of these lineages takes hold and becomes an important part of an outbreak in any location. The authors attempt to separate out these effects but have inadequate evidence to say anything conclusive.
“If the ‘strain’ in question were substantially more transmissible than others, it would rapidly become very obvious due to the nature of exponential growth – if two things are growing exponentially but at substantially different rates, the one with a higher rate will grow much more quickly than the one with the lower rate. This has not happened so any difference in transmissibility, if it exists, must be small.”
No conflict of interest.
Dr Jemma Geoghegan, Virologist, Senior Lecturer, University of Otago, comments:
“When a virus replicates it often makes mistakes, or mutations. Most mutations are neutral and have no or little effect on the function of a virus, or alter its transmissibility or the severity of the disease it causes. Sometimes, however, mutations can influence the way a virus infects its host.
“There are hundreds of mutations that have been detected in the genomes of SARS-CoV-2. One mutation that people are paying close attention to is called D614G, which is a mutation in the spike protein (the amino acid D changed to a G at position 614). It has been suggested that this mutation has led to an increase in the virus’ transmissibility.
“The problem with drawing this conclusion is that this mutation first occurred in the founding virus types in Europe. It is likely, then, that this variant of the virus with a G amino acid just got lucky and due to the ‘founder effect’ it increased in frequency – i.e., the virus got there first and so started spreading first. The virus variant with a D amino acid remains more frequent in Asia, where the virus first broke out. Countries like New Zealand have about a 50:50 mix of each type – that’s because we have had many incursions of the virus from different parts of the world.
“It is not yet possible to say whether the mutation has caused an increase in transmissibility. To make such a conclusion, researchers would need to conduct experiments using cell culture and/or animal models in the lab.
“As for a vaccine, it is important to monitor any changes in the virus’ genome that are increasing in frequency. The spike protein is particularly important for any potential therapeutics, so it is worth monitoring mutations in this region carefully.”
No conflict of interest.
Dr Matloob Husain, Senior Lecturer in Virology, Department of Microbiology and Immunology, University of Otago, comments:
“Just like influenza, SARS 2.0 is one of the RNA viruses which are notorious for evolution in the host. When a RNA virus is novel (like SARS 2.0) and the population is naïve (doesn’t have pre-existing immunity), it spreads fast among the population (this is what happening in SARS 2.0 case). During its spread, a virus may mutate to adapt better in the population. Basically, this is what the paper in question is informing.
“They have identified particularly one prevalent mutation (D614G) in the spike protein which would be the target of many vaccines under development; this mutation could be detrimental to the efficacy of those vaccines. However, with the methods they have used, it is difficult to conclude that the circulating virus with this mutation is more contagious/pathogenic.
“Constant evolution is the main reason behind recurring seasonal influenza epidemics and need for flu vaccination every year; we may see the same with SARS 2.0 if it keeps circulating and evolving.”
No conflict of interest.
Associate Professor James Ussher, Department of Microbiology and Immunology, University of Otago, comments:
“This is an interesting paper. It seems that the D614G mutation in the spike protein is becoming more frequent over time and is spreading geographically. It does not seem to be associated with more severe disease but may be associated with increased transmission. The effects on transmission, however, will need to be confirmed in experiments in the laboratory (in vitro cell culture and animal models).
“It is uncertain at this time what impact this might have on vaccine development. The mutation is in an area of the spike protein that has previously been shown to be a target of antibody responses. However, it is not in the area of the spike protein that is involved with binding to its receptor (the receptor binding domain), ACE2. Most vaccine strategies are targeting the spike protein, trying to induce antibodies that bind to the receptor binding domain, preventing viral entry. This paper identified very few mutations to date in the receptor binding domain, which is encouraging for vaccine design. Laboratory experiments are required to define the impact, if any, of the D614G mutation on immune escape.”
No conflict of interest.